12 Critical Diabetes Skin Warning Signs Every Person Should Recognize
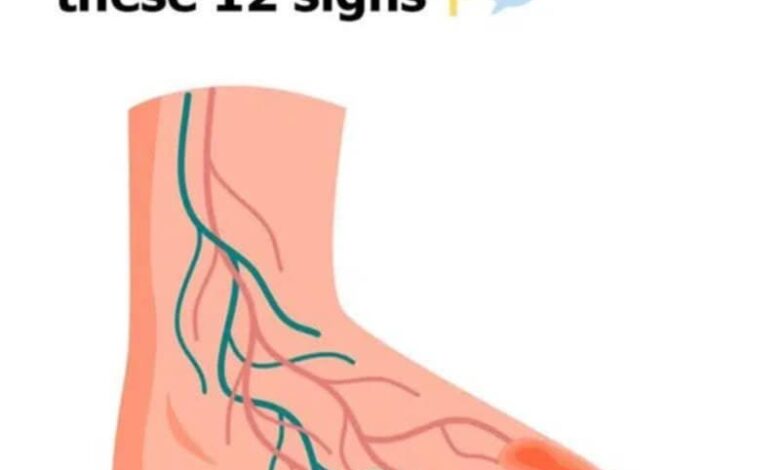
Have you noticed unusual changes in your skin that seem unexplainable? For individuals with diabetes or those at risk of developing this condition, the skin often functions as an early detection system, providing valuable insights about blood glucose management and insulin function. Understanding these diabetes-related skin conditions is crucial because early identification can significantly impact successful long-term health management.
Medical research reveals that approximately one-third of people with diabetes will develop a skin-related condition during their lifetime. This comprehensive health guide examines 12 important diabetic skin conditions that require immediate attention and proper medical evaluation.
From distinctive dark patches to wounds that heal slowly, this complete wellness resource explains each condition and its potential implications for your overall health. By learning to identify these diabetes warning signs on your skin, you’ll be better prepared to take proactive steps and seek appropriate medical care, potentially preventing more serious health complications.
Understanding Diabetes-Related Skin Conditions
Diabetes affects the body in numerous ways, and skin health often serves as an important indicator of underlying metabolic issues. Many conditions associated with diabetes, such as necrobiosis lipoidica (characterized by raised, shiny skin patches) or acanthosis nigricans (presenting as darkened, velvety areas typically around the neck and joint areas), are clear indicators of elevated blood sugar levels and insulin resistance.
Individuals with diabetes may also experience digital sclerosis, where fingers become stiff and less flexible, and diabetic blisters that appear similar to burn injuries but occur without any trauma or injury.
Skin infections represent a significant concern for people with diabetes due to compromised immune system function. Fungal infections including athlete’s foot and other moisture-related conditions tend to develop more frequently in diabetes patients.
Diabetic dermopathy creates distinctive light brown, scaly patches commonly found on the lower legs, often referred to as “shin spots” in medical terminology. Additional symptoms include eruptive xanthomatosis, which presents as yellowish bumps surrounded by red areas, particularly when blood sugar control is inadequate.
1. Necrobiosis Lipoidica: Recognizing the Warning Signs
Necrobiosis Lipoidica manifests as distinctive reddish, yellowish, or brown patches that may initially appear as small, firm bumps on the skin. These initial bumps are typically just the beginning of a more extensive skin condition that requires medical attention.
Over time, these bumps develop into thickened patches that most commonly appear on the legs. The affected skin areas often take on a distinctive porcelain-like appearance, making small blood vessels beneath the skin surface clearly visible to observers.
These patches may cause itching or inflammation and can go through periods of activity and remission. While having diabetes doesn’t guarantee the development of this condition, it occurs more frequently in individuals with diabetes. Regular skin monitoring and early detection are essential for managing these symptoms effectively.
Understanding necrobiosis lipoidica is important for comprehensive diabetes management, as it can provide valuable information about blood sugar control and overall health status.
2. Acanthosis Nigricans: Dark Skin Patches and Insulin Resistance
Acanthosis Nigricans is a skin condition that often indicates potential issues with insulin processing in the body. This condition presents as darker, velvety patches of skin that typically appear in body fold areas such as the neck, armpits, and other skin creases.
The presence of these darkened areas may indicate increasing insulin resistance in the body, which is often a precursor to type 2 diabetes development. Recognizing these changes early can prompt individuals to take preventive health measures before blood glucose levels become more difficult to manage.
Identifying Acanthosis Nigricans extends beyond cosmetic concerns; it serves as an important health indicator that may suggest prediabetes or undiagnosed diabetes mellitus. These warning signs should not be ignored, as they encourage individuals to seek medical testing and potentially make lifestyle adjustments or seek professional medical guidance.
Early intervention based on recognizing these skin changes can significantly improve long-term health outcomes and diabetes prevention strategies.
3. Digital Sclerosis: When Skin Becomes Thick and Stiff
While acanthosis nigricans often indicates elevated insulin levels, digital sclerosis presents a different warning sign for individuals managing diabetes. This skin complication causes skin thickening and reduced elasticity, leading to joint stiffness and decreased mobility.
The hands are frequently affected areas, where fingers can become so rigid that performing simple daily tasks becomes challenging and uncomfortable.
Maintaining optimal blood glucose control is essential for addressing digital sclerosis symptoms. Keeping diabetes well-managed may help reduce symptoms, with some patients experiencing improvement through specific nutritional supplements like alpha-lipoic acid or targeted physical therapy exercises designed to improve flexibility and range of motion.
Paying attention to these symptoms is crucial for preventing additional complications and maintaining quality of life while managing diabetes effectively.
4. Diabetic Blisters (Bullosis Diabeticorum): Unexpected Skin Formations
Diabetic blisters may appear suddenly and unexpectedly on the skin, often causing concern for individuals who notice them. These bubble-like formations can develop without warning on feet, forearms, legs, or hands, resembling burn blisters but occurring without heat exposure or injury.
Interestingly, these blisters typically don’t cause significant pain or discomfort, despite their alarming appearance. However, proper care and medical attention are essential when these formations appear.
The appearance of diabetic blisters can be concerning, especially considering that open wounds and diabetes management require careful attention due to increased infection risk and complications related to diabetic neuropathy and circulation issues.
Medical consultation is important for any unexpected skin changes. Healthcare providers may recommend protective measures or prescribe treatments that prevent complications and promote proper healing while minimizing infection risks.
5. Skin Infections: Common Complications in Diabetes
Building on concerns about diabetic blisters, skin infections represent another significant complication faced by individuals with diabetes. These conditions often manifest as warm, swollen skin areas that may feel tender or painful and frequently show symptoms like itchy rashes or small blister formations.
Yeast infections caused by Candida albicans are particularly common among people with diabetes due to elevated sugar levels that provide ideal conditions for yeast growth and proliferation.
Proper skin care is essential for managing infections, especially since they commonly develop between toes, around nail areas, or on the scalp—locations prone to moisture retention and fungal growth conditions that support athlete’s foot and ringworm development.
Maintaining clean, dry conditions in affected areas helps prevent further complications. Since diabetes patients may require more intensive treatment approaches, including extended antibiotic or antifungal medication courses, prompt healthcare consultation can prevent infection progression and serious complications.
6. Shin Spots (Diabetic Dermopathy): Light Brown Patches
Shin spots represent a frequent yet often overlooked indicator of diabetes. These patches appear as light brown, scaly marks that may resemble age spots but actually indicate underlying diabetes-related changes in the body.
They typically appear on the shin areas and may include slight indentations in the skin surface. While these spots usually don’t cause discomfort or pain, their presence provides important information about diabetes management effectiveness.
Many individuals with shin spots don’t realize they have them since they typically don’t cause symptoms like itching or pain. Despite the lack of discomfort, recognizing these indicators is important because they reflect blood vessel damage caused by elevated sugar levels over extended periods.
The positive aspect is that most shin spots gradually fade when blood sugar levels achieve better control; however, persistently high sugar levels may result in longer-lasting skin markings.
7. Eruptive Xanthomatosis: Yellow Bumps and Blood Sugar Control
Moving beyond shin spots, eruptive xanthomatosis represents another skin condition that may develop in individuals managing diabetes. This condition appears as small, reddish-yellow bumps that can emerge on various body parts including thighs, buttocks, elbows, or behind the knees.
These bumps initially resemble pimples but quickly develop a distinctive yellow coloration that sets them apart from typical skin blemishes.
These formations don’t remain passive; they often itch and feel tender when touched, causing noticeable discomfort for affected individuals. When skin develops these distinctive bumps, it often indicates that blood sugar levels require closer monitoring and management.
Fortunately, with consistent diabetes control and appropriate treatment strategies, these skin irritations typically resolve quickly, allowing skin to return to its normal appearance without long-term complications.
8. Granuloma Annulare: Distinctive Ring Patterns
Transitioning from eruptive xanthomatosis, granuloma annulare represents another skin condition that can concern individuals with diabetes. This disorder presents as raised bumps that may appear red or match natural skin tone, with patches potentially showing bluish, pink, or purple coloration.
While the exact connection between granuloma annulare and diabetes isn’t completely understood, people with diabetes seem to experience this condition more frequently than the general population.
Granuloma annulare often resolves spontaneously and may prompt healthcare providers to evaluate for underlying diabetes. If you notice these characteristic ring or arc-like patterns on your skin, discussing them with a healthcare professional is advisable.
Although these formations can be persistent and may recur after treatment, management options such as light therapy or topical steroid treatments may be recommended to address symptoms effectively.
Continue reading on next page…